Lumbar discectomy
This is now a common and routine procedure. The aim of this operation is to remove some of the disc to relieve pressure on the nerves. Before this I will have encouraged you to consider other options. Over 90% of disc prolapses settle down by themselves with simple pain killers and exercises. Yours is obviously causing significant problems or other measures have failed to work. I will not remove all of the disc. The disc is an important stabiliser of the spine and if I was to remove it all a further procedure would have to be performed to stabilise the spine.
Before the operation
You will be contacted by the hospital and invited to come for a pre-assessment. You will have some routine blood tests and have your pulse and blood pressure checked. You may also need to have an electric tracing of your heart activity. You will need to come into hospital on the day of your surgery. When you come in the nurses will check that you are ready for your surgery and will fit stockings on your legs to reduce the risk of getting a deep vein thrombosis. I will visit you in your room and check that you are prepared to have your surgery. You will also be visited by the anaesthetist who will review all the tests that you have had and discuss that anaesthetic with you. You will be escorted down to the operating theatre. Your anaesthetic will be administered and you will then be asleep.
The Operation
We will carefully position you on to your front. Based on an x-ray I will localise the level that we will be operating at. The skin will be cleaned with a spirit to reduce the number of bacteria on the skin and reduce the risk of infection. An antibiotic will also be given to do this. A small cut will be made in the middle of your back. The cut will be deepened through the fat and a cut will be made into the covering layer of the muscle. The muscle is then peeled away from the spine to expose the bones. A small window is created by removing the ligament between the bones and some of the bone if necessary. Through this window I will be able to see the nerves and move them out of the way. THe disc is behind this. I will check that I am operating at the correct level again to be certain that I am at the correct level. A small cut will be made in the disc and special instruments will be used to remove the soft part of the disc that is pushing backwards onto the nerves. I will wash out the are to ensure that there are no loose pieces of disc within the disc that could come out later to cause further pressure on the nerves. Once I have cleared away as much of the disc as is needed I will explore the route of the nerve as it leaves the spine. Often some disc material is squeezed out along this route and this needs to be cleared too to be certain that the operation will be a success. I will then give you an epidural to reduce the pain of the operation. I will inject a gel that is designed to try to reduce the chance of scar tissue formation. I will then stitch up the small hole in layers. A stitch will be buried under the skin and paper stitches will be used. This will all be covered with a waterproof dressing.
|
|
|
|
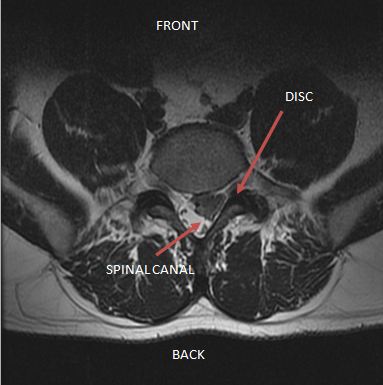
MRI scan image showing a large disc prolapse compressing
the sac that contains nerves and spinal fluid
|
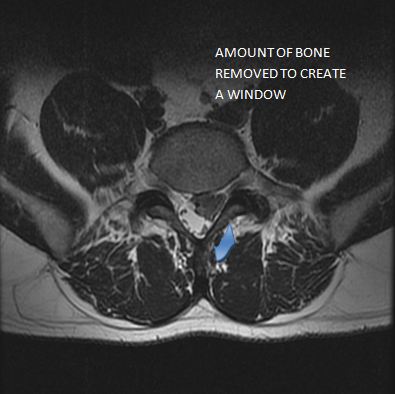
The same MRI Scan image showing the amount of bone that
may need to be removed to create a window
|
Risks
The operation is designed to relieve your leg pain. Although this is a routine procedure it is important to be aware of the risks involved.
-
Infection. Surgery always carries with it a risk of infection although this is rare. This may lead to a temporary increase in back pain and an antibiotic may need to be prescribed. An increase in back pain may occur for up to a year may be permanent. The risks of infection are approximately 1%.
-
Damage to nerves. Numbness, pins and needles and weakness may improve after surgery but recovery may be slow. If there are severe symptoms before surgery, there may be some ongoing numbness and weakness after the operation which if the nerve has been permanently damaged may not recover. On very rare occasions, the nerve may be damaged at the time of the operation leading to an increase in pins and needles, numbness and weakness. This happens in less than 1% of patients.
-
Damage to the nerves to the bladder and bowel and both legs ( Cauda Equina Syndrome) This is extremely rare and happens in less than 1% of spinal surgery.
-
Dural tear. A tear to the lining of the sac containing the nerves (dura) can cause a nasty headache. This is due to a small leak of the fluid that surrounds the nerves and brain. The tear is stitched or patched during the surgery and you may have to lay flat for a while after the operation to allow it to seal over. It can cause headaches which may last for a few days but should wear off completely. It does not seem to change the final outcome of the surgery.
-
Ongoing back pain. On occasions, back pain can be the same or even a little worse after back surgery. The main aim of spinal decompression surgery is to improve your leg pain.
-
Recurrance. Not all the disc is removed and it is possible that if you damage your disc that a further piece of it may break or detach and protrude, herniated or bulge out into the spinal canal and press on a nerve.
-
Wrong level. The incision or cut that is made in your back is quite small and it would be easy to be operating at the wrong level of the spine as the bones look very similar. That is why I take multiple x-rays during the operation to be sure that I am working at the correct level.
Risks Related to Anaesthetics
Modern anaesthetics are extremely safe. However, as with all general anaesthetics, there is a very small risk of complication concerning the anaesthetic during the procedure. Any existing medical conditions will be taken into consideration.
General Risks
There are a number of complications that can occur in any operation e.g. blood clots, heart attacks, and chest infections. The risk of these complications in a person of average good health is low. If you have any medical conditions or are taking any medicines it is very important that you inform the pre-assessment nurse, surgeon and the anaesthetist. Constipation is common after any spinal surgery and I will encourage you to take laxatives if you have any difficulty opening your bowels. Some people find that they are left with a tender scar, to prevent this I will suggest that once the wound has healed, at about two weeks, you start to massage the scar itself. You can use a cream or oil if you want.
After the Procedure.
You will then be placed back in your bed, woken up and taken to the recovery area. Here your pulse, blood pressure and breathing will be closely monitored. Once the staff are sure that you have woken up fully from the anaesthetic and that your pain is well controlled they will organise for you to transferred back to the ward. Later the same day either the physiotherapists, nurses or myself will get you out of bed and start you standing and walking. So long as you have fully recovered from the anaesthetic and your blood pressure is normal, we will encourage you to walk.
Although it may even be the same day, it is usually the next day that the physiotherapists will ensure that you are able to walk a reasonable distance and safely manage the stairs. Once you have done this you will be ready to go home. By the first day after the operation the epidural that I gave you during the operation may have worn off and you may notice more pain. Do not be surprised that you have more pain now compared to directly after the operation. With the epidural wearing off and that fact that you are now moving about, it is only natural for your back to hurt. Hopefully you will notice a difference in your leg pain. Remember not everyone notices this difference straight away. Remember that the operation is mainly to try to get rid of your leg pain and any numbness, weakness or pins and needles that you have may recover slowly. There is no guarantee of this recovery and only time will tell if once the pressure is removed from the nerves, whether the nerve will fully recover. The physiotherapists will go through the exercises that you can do.
THE FIRST WEEK
Pain relief
-
A local anaesthetic is injected into the wound at the time of surgery, which should help with pain relief.
-
You will be given painkillers as required on the ward and for you to take home if needed.
-
It is important to start moving and if pain is preventing you from doing this let us know and we may be able to alter you pain medication to help you to be able to become independent.
-
You may find that your leg pain is still very much the same as before. In some cases the nerve irritation does take a while to settle down. In addition you will have the pain of the operation. Although this is a different pain you may find that you need to take just as many pain killers as before to keep this under control. Do not expect to be completely pain free.
-
If you do not feel significant pain it may still be important to take the pain killers that you have been given. It is better that while you are increasing your level of activity you do not feel inhibited by increasing pain.
BED MOBILITY AND EXERCISES
-
You can lie on your side if you wish. Whichever position is most comfortable to allow you to sleep well is fine.
-
Whilst in bed, you can lie on your side or sit slightly propped up as comfort allows.
-
Early mobility is very important and the physiotherapists will start you walking within 24 hours of surgery, the same day if possible. You will also be encouraged with your exercise programme.
-
You will be encouraged to be as mobile as possible. This will include going up and down stairs within a couple of days of surgery.
-
Generally if it is comfortable to do it is safe to do. Remember to build up gradually.
DISCHARGE HOME
-
Discharge from hospital is normally within 1-3 days after your operation.
-
You will be given a sheet of exercises by the physiotherapists to continue at home. If you are comfortable you can increase these, but build up in small amounts. It is a slow recovery and is not meant to be a race.
-
Becoming constipated is painful after back operations. Take laxatives as necessary.
WEEKS 2 - 6
For the first couple of weeks it is recommended that you avoid:
-
Sitting in low chairs you will do no harm but it may increase your back pain.
-
Sitting for a long time – for example longer than 20 minutes. The length of time that you will be able to sit and stand for will gradually get longer over this time.
-
Getting into the bath until your wound is clean and dry.
-
Driving for the 2-4 weeks – you can be a passenger for short journeys.
-
Prolonged rest – you will get stiff and your muscles will get weaker.
Return to Normal Activity
It is vital that you play an active part in your recovery. You may feel some discomfort but you are not harming yourself. Your exercises will help you return to normal more quickly and to feel better in yourself. It is quite safe to take painkillers to help you to do this. If leg pain recurs, you should ease off and rest until symptoms settle. Gradually increase the level of strenuous activity and lifting and generally by 3 months you should be back to normal.
Housework
-
You can start back to normal activities, as you feel able to do so.
-
You may want to ask someone else to do the hoovering in the early stages.
-
Avoid lifting heavy furniture.
-
After 12 weeks it is expected that you can lift as you normally would do but use your common sense.
Return to work
-
If your job involves sitting at a desk, you may return after 2- 6 weeks, depending on how you are progressing. It is often possible to return to working from home with reduced hours as early as 2 weeks. Working from home or for reduced hours and lighter duties are ways that you may be able to return to work sooner and should be discussed with your employer.
-
Your ability to get to work, such as being able to drive a car, and how long you can sit for any length of time may actually determine when you can return to work.
-
If your job involves heavy lifting, you may need to delay your return for 3 months. It is recommended that you discuss your job with the Consultant.
Sport
Sexual Activity
YOU SHOULD CONTACT US IF YOU EXPERIENCE ANY OF THE FOLLOWING AFTER YOUR OPERATION:
- A loss of sensation or change in your ability to move your bowels or empty your bladder.
- Any significant leg pains and pins and needles.
- Any redness, oozing or discharge from your wound.
- Feeling unwell with a raised temperature.
REMEMBER
It is normal to feel some discomfort after your operation and this is not harmful
Try to do your exercises and walking on a little and often basis every day with short rests as necessary
Recovery times can vary – research has shown that by doing exercises you can improve the short and long termoutcome of your operation and have less need for further medical intervention.